Clinical Data Management: Pioneering Excellence in Health, Life, and Pharma Sciences
The life science, health science, and pharmaceutical industries are among the most rigorously regulated sectors globally, prioritizing patient safety during clinical trials and post-marketing phases. Compliance with country-specific regulations set by regulatory bodies is mandatory for all trials. Adhering to regulations like Good Laboratory Practice (GLP), Good Clinical Practice (GCP), and CFR Part 11 is essential when introducing new products to the market.
Clinical data, which includes information for developing and maintaining software systems, databases, processes, and protocols, is crucial for these studies.
Ensuring Data Integrity in Clinical Research
Clinical Data Management (CDM) ensures data integrity throughout the research process, making sure datasets are accurate, secure, reliable, and ready for analysis. By using a systematic process, a CDM team is responsible for collecting, entering, cleaning, and processing information gathered during a clinical research project.
This ensures the accuracy, completeness, and consistency of the clinical trial data while adhering to regulatory standards and guidelines.
Training Programs in Clinical Data Management
The Bangalore Clinical Research Institute (BCRI) is known for offering various training programs in clinical research and related fields, including Clinical Data Management (CDM). The CDM training is designed to provide participants with the skills and knowledge required to manage clinical trial data efficiently, ensuring compliance with industry standards and regulatory guidelines.
The main goal of CDM is to ensure the validity and reliability of the data, so it’s ready for regulatory submission and subsequent analysis. It serves as the backbone for producing high-quality, statistically sound results that inform medical decisions and regulatory approvals.
Advantages of CDM Training
Undertaking Clinical Data Management (CDM) training from reputable clinical research institutes offers a range of benefits, especially for individuals aspiring to build a career in clinical research or related fields. Regulatory affairs and compliance are fundamental aspects of CDM, ensuring that all collected data adheres to stringent regulatory standards and guidelines set by authorities such as the FDA and EMA.
By maintaining records and implementing robust validation processes, CDM guarantees that the data adheres to regulatory requirements to not only facilitate the approval process for new treatments and interventions but also to uphold the integrity of the research.
High-quality data ensures that the results of clinical trials are statistically sound and dependable, forming a solid foundation for medical decisions and ultimately advancing patient care.
Responsibilities in Clinical Data Management
Ensuring Data Quality and Integrity
CDM ensures that the results of clinical trials are statistically sound and dependable, forming a solid foundation for medical decisions and ultimately advancing patient care.
Compliance with Regulatory Standards
Maintaining records and implementing robust validation processes guarantees that the data adheres to regulatory requirements, facilitating the approval process for new treatments and interventions.
Data Collection and Management
CDM involves the systematic collection and management of data, ensuring its accuracy and reliability.
Facilitating Accurate Analysis and Reporting
By ensuring data quality and integrity, CDM facilitates accurate analysis and reporting, which are crucial for regulatory submissions and medical decision-making.
Role of Clinical Data Managers
The Data Manager will manage the clinical trial data collection, processing, and analysis. Clinical Data Managers work closely with clinical research team members, including clinical research associates, medical monitors, pharmacovigilance, and biostatisticians to ensure that all aspects of the data management process are executed efficiently and accurately.
Main Activities in Clinical Data Management
- Data Management Plan (DMP) Development
- Database Design and Setup
- Data Capture
- Data Validation
- Discrepancy Management
- Medical Coding
- Database Lock
Essential Skills for Effective Clinical Data Managers
Here are some essential skills for Data Managers to ensure the successful capture, cleaning, and lock of clinical trial data, contributing to the efficacy and effectiveness of clinical research outcomes:
- Technical Proficiency
- Analytical Skills
- Attention to Detail
- Regulatory and Compliance Knowledge
- Communication and Collaboration
- Project Management Skills
- Quality Control and Assurance
- Ethical and Confidentiality Awareness
Roles Involved in Clinical Data Management (CDM)
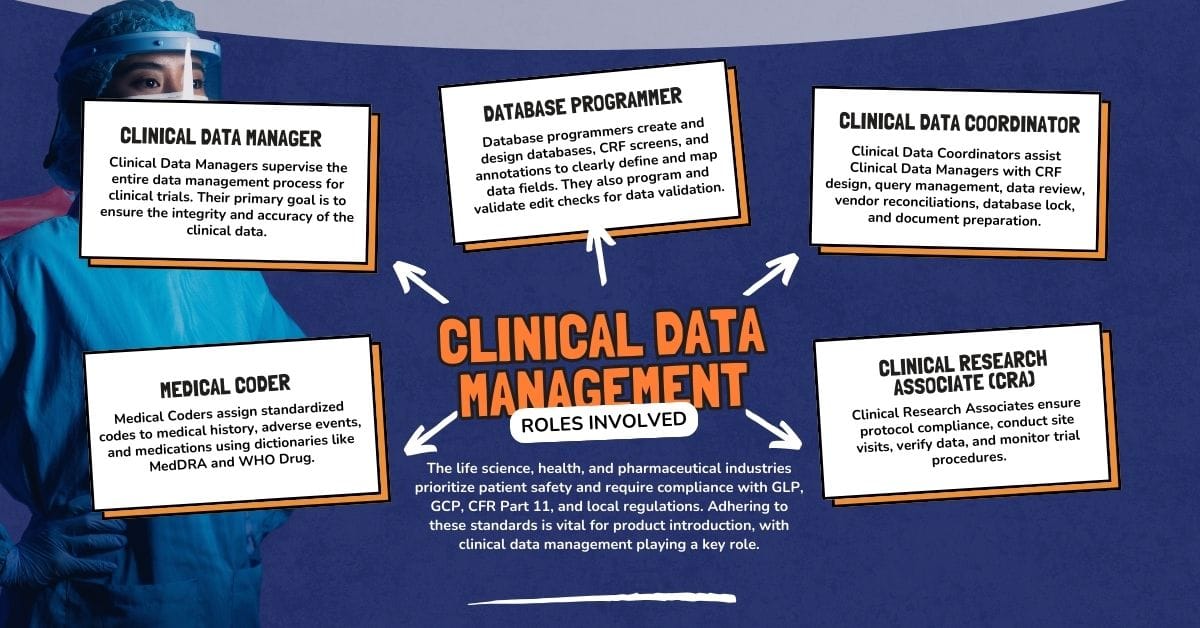
Clinical Data Manager
Clinical Data Managers supervise the entire data management process for clinical trials. Their primary goal is to ensure the integrity and accuracy of the clinical data.
Database Programmer
Database programmers create the database, design Case Report Form (CRF) screens, perform CRF annotations to ensure that data fields are clearly defined and mapped to the database, program, and validate the edit checks for data validation.
Clinical Data Coordinator
Clinical Data Coordinators assist Clinical Data Managers with data management-related activities like CRF designing, query management, data review, vendor reconciliations, database lock, and support in preparation of data management documents.
Medical Coder
Medical Coders review and code variations such as medical history, adverse events, and medications into standardized codes using coding dictionaries like MedDRA (Medical Dictionary for Regulatory Activities) and WHO Drug (World Health Organization Drug Dictionary).
Clinical Research Associate (CRA)
Clinical Research Associates monitor the clinical trials process to ensure compliance with study protocol, conduct site visits, and perform source data verification. They ensure the clinical trials run smoothly, monitoring all procedures, processes, and results, ensuring the researchers follow established guidelines and protocols every step of the way.
Investigator
Investigators are responsible for the conduct and oversight of clinical trials at their respective sites.
Clinical Research Coordinator (CRC)
Clinical Research Coordinators manage the day-to-day operations of clinical trials at the study site. They handle patient recruitment, informed consent, data collection, and adherence to the study protocol. They are responsible for entering data from Case Report Forms (CRFs) into electronic databases.
Biostatistician
Biostatisticians (SAS Programmers) are responsible for designing the statistical aspect of clinical trials and analyzing the study data.
Medical Writer
Medical Writers are responsible for creating and maintaining a wide spectrum of documents such as protocol writing, investigator’s brochures, informed consent forms, clinical study reports, regulatory submissions, and scientific publications.
Stages of Clinical Data Management

Start-up Stage
The study start-up phase in clinical data management involves planning and preparation for the data collection, processing, and analysis of data in a clinical trial or study. The Start-up phase consists of activities like:
- Interpreting Protocol: Review the protocol to understand the study’s primary objectives, secondary objectives, safety endpoints, and data requirements.
- Development of Data Management Plan (DMP): The Data Management Plan (DMP) is a comprehensive document that outlines all data management activities, standards, and procedures for a clinical trial. It details the processes, standards, and responsibilities necessary to ensure data integrity and compliance with regulatory requirements.
- CRF Design and Development: Designing Case Report Forms (CRFs) or electronic CRFs (eCRFs) as per protocol requirements to capture all required data systematically.
- Database Design and Development: Developing the clinical database to store and manage collected data. This process ensures that the database is built according to protocol requirements and regulatory standards, ensuring data accuracy, integrity, and accessibility. Key activities involved in developing the database design are:
- Creating Database Specifications: Database specifications detail the requirements and structure of the database, serving as a blueprint for its development.
- Designing the Database: The database is developed based on the specifications provided in the database specification document within the Clinical Data Management System (CDMS) such as Medidata Rave, Clinevo, Veeva, Inform, etc.
- Edit Check Specification Development: Edit checks are automated validation checks applied to data entry to ensure data quality, consistency, and integrity throughout a clinical trial or study. These checks are designed to flag errors or inconsistencies in the data at the point of entry, thereby facilitating the correction and maintaining the accuracy of the dataset. Some examples of edit checks are range checks, mandatory fields checks, data format checks, future date checks, cross-form checks, duplicate checks, and logical checks.
- Testing the Database: This ensures it functions correctly, meets protocol requirements, and adheres to regulatory standards. Key activities involved in testing the database are:
- Database Modules Testing: Testing individual components such as CRF forms, fields, visits, dynamics, roles, and derivations to ensure they function as expected and verifying each field captures data correctly as expected.
- Edit Check Testing: Testing of edit checks to ensure edit checks function as intended without generating false positives or missing errors.
- Medical Coding: Testing individual components of the medical coding process to ensure they function correctly and to ensure that coding logic accurately maps clinical terms to standardized codes.
- Integration: Testing the interactions between integrated components or modules to ensure they work as expected. Some examples of integrations system testing are ePRO, eCOA, lab modules, and safety gateway.
- Audit Trail: Audit trail testing is performed to ensure that all changes to data are accurately recorded, preserving the original data and documenting modifications with accurate and precise timestamps.
- User Acceptance Testing (UAT): Conducting UAT with end users such as Data Managers, Medical Coders, Clinical Research Associates (CRAs), and external stakeholders to ensure the database meets their needs and expectations. Collecting feedback from end users, identifying any issues or areas for improvement, and making the necessary adjustments or updates to the database based on user input.
- Validation and Documentation: Documenting all testing procedures, results, and any modifications made to the database and ensuring the database design and testing processes are fully documented to meet regulatory requirements.
- eCRF Completion Guidelines: This provides detailed instructions for completing electronic Case Report Forms (eCRFs), ensuring consistent and accurate data entry across all study sites.
- Data Validation Plan The Data Validation Plan outlines the procedures and criteria for validating the data collected during the clinical trial.
- Data Transfer Agreement/Specification Specifications for external vendors outline the requirements and expectations for third-party service providers involved in the clinical trial, such as laboratory services, eCOA, and ePRO.
Conduct Stage
The conduct phase is a critical period in the clinical trial lifecycle, focusing on the accurate collection and monitoring of clinical trial data to support study outcomes and regulatory requirements. This phase consists of several key activities:
Data Collection and Entry
Data collection involves gathering information from various sources such as patient records, laboratory tests, and clinical observations during a clinical trial. Modern CDM systems often use Electronic Data Capture (EDC) tools to streamline data collection. EDC systems reduce errors associated with manual data entry, enhance data accuracy, and facilitate real-time data access.
Data Cleaning and Validation
The data cleaning and validation stage involves a meticulous process to ensure data integrity and readiness for analysis. By effectively managing queries, reviewing data, reconciling external vendor data, SAE reconciliation, and medical coding, clinical data management teams can uphold the highest standards of data quality. These activities are essential for generating reliable and credible results in clinical research, supporting regulatory submissions, and contributing to advancements in medical research and patient care. Key activities include:
- Discrepancy Management: Identifying, generating, and resolving queries related to discrepancies, inconsistencies, missing data, or errors in the collected data.
- Data Review: Regularly reviewing entered data and performing quality checks to ensure accuracy, completeness, and compliance with protocol requirements.
- SAE Reconciliation: Ensuring that all Serious Adverse Events (SAEs) reported in the clinical database are consistent with those reported in the safety database by comparing and addressing discrepancies. Documenting the reconciliation process, including discrepancies identified, queries raised, and resolutions, is crucial for audit trails and regulatory inspections.
- External Vendor Reconciliation: Reviewing and reconciling data from the clinical database with data from external vendors such as central laboratories or electronic patient-reported outcomes (ePRO) to ensure data consistency and completeness by identifying discrepancies and resolving differences.
- Medical Coding Using MedRA and WHODDE Dictionaries: Classifying multiple verbatim terms using a validated medical dictionary supplied by the customer under license by the relevant licensing bodies (MSSO, Uppsala) to produce a statistically quantifiable count of all similar terms in a clinical database.
Closeout Stage
Once the study enters the last patient’s last visit, the study close-out process begins. This phase involves several key activities aimed at ensuring the completeness, accuracy, and integrity of the collected data and preparing for study closure and regulatory submission. Each of these closeout phase activities plays a crucial role in the overall clinical data management process. The closeout stage consists of the following activities:
Database Quality Control
This process involves a detailed review of all data entries to ensure accuracy, completeness, and consistency. Quality control processes include final data review, addressing any remaining discrepancies, and confirming that all data points are correctly captured in the clinical database.
Medical Coding Review and Approval
During the closeout phase, final medical coding review and approval are conducted to ensure that all terms are accurately coded and consistent with regulatory standards.
SAE Reconciliation and Approval
The final SAE reconciliation process involves verifying that all reported SAEs are correctly documented and reconciled between the clinical and safety databases. Approval of this reconciliation ensures that all safety data is accurate and complete.
Database Lock Activities
Closing or locking the database is fundamental for preventing inadvertent or unauthorized access to the data. The data manager will initiate and complete the database lock checklist and perform quality control checks to ensure the database is ready for locking.
Once all necessary approvals for the database lock are in place, the process of locking the database can proceed. The database lock signifies that the data is ready for final analysis and regulatory submission.
Post-Lock Data Extract and Transfer
After the database is locked, data extracts are performed for final analysis and reporting. This involves securely and accurately transferring data to statistical analysis systems (SAS) or external stakeholders while maintaining the integrity of the dataset.
Data Archiving
Data archiving is the process of securely storing all trial-related data and documentation. This ensures that the data remains accessible and intact for future reference and regulatory inspections.
Decommissioning Activities
Decommissioning involves the systematic shutdown of study systems and applications used during the clinical trial. This includes securely transferring study media to sponsors and sites, archiving all data, removing the systems from active use, and retiring systems in accordance with organizational and regulatory guidelines.
The Role of CDASH and CDISC in Clinical Data Management
To further enhance the effectiveness and reliability of clinical data management, industry standards such as CDASH (Clinical Data Acquisition Standards Harmonization) and CDISC (Clinical Data Interchange Standards Consortium) play a pivotal role.
These standards ensure that data collected during clinical trials is consistent, accurate, and easily interpretable, thus supporting regulatory compliance and facilitating seamless data integration and analysis.
What is a Clinical Data Management System?
A Clinical Data Management System (CDMS) is a tool used in clinical research to manage the data of a clinical trial. These systems ensure data accuracy, integrity, and compliance with regulatory requirements. Key components of a CDMS include:
- Database Management
- Data Cleaning and Validation
- Data Integration
- Reporting and Analysis
- Audit Trails
- Security Features
Tools Used in CDMS
- Electronic Data Capture (EDC): EDC systems streamline the process of collecting and managing clinical trial data electronically, replacing traditional paper methods. This transition to digital data capture offers numerous advantages, including improved data accuracy, real-time access to data, and enhanced regulatory compliance.
Common EDC systems include Medidata Rave, Clinevo, Oracle Clinical, Veeva, Merative, and Veidoc.
- Electronic Patient Reported Outcomes (ePRO): ePRO systems allow patients to record and submit their health outcomes digitally in real time using devices such as smartphones, tablets, or computers.
- Interactive Response Technology (IRT): IRT systems manage patient enrollment, randomization, and drug dispensation in clinical trials.
- Randomization and Trial Supply Management (RTSM): RTSM systems manage patient randomization and the supply of investigational products during clinical trials.
- Safety Gateway: Safety gateway systems are integral in managing and reporting adverse events. These systems streamline the collection, assessment, and regulatory reporting of safety information, ensuring safety concerns are promptly addressed and regulatory requirements are met.
- Coding Application: Coding systems standardize the classification of medical terms used in clinical trials, such as adverse events and medication.
- Laboratory Data Integration: Lab modules integration systems ensure that lab data is seamlessly transferred and managed within the clinical trial database, maintaining data integrity and compliance.
The Future of Clinical Data Management
With technological advancements like artificial intelligence (AI), machine learning (ML), and medical devices, CDM is undergoing a significant transformation towards a digital age of real-time data collection and management. Clinical data management systems will need to adapt to manage diverse data sources and ensure seamless integration and consistency across decentralized trial frameworks.
The future of clinical data management is poised to be shaped by several trends and technologies:
- Artificial Intelligence and Machine Learning
- Patient-Centric Data Collection
- Cloud Computing and Big Data Analytics
- Decentralized Clinical Trials (DCTs)
Training and Career Advancement in Clinical Data Management
Training from a reputed clinical research institute ensures you gain the knowledge, skills, and certification needed to excel in Clinical Data Management. It provides a structured learning pathway, hands-on experience, and access to a strong professional network, all of which are invaluable for building a successful career in the field. Key benefits of such training include:
Industry-Relevant Curriculum
Training programs are designed to align with industry standards such as ICH-GCP and CDISC (SDTM, ADaM). Courses focus on practical and theoretical knowledge, ensuring students are well-prepared for real-world challenges.
Hands-On Experience
Institutes often provide hands-on training with industry-standard software like Medidata Rave, Clinevo, Oracle Clinical, REDCap, and others. This includes exposure to Electronic Data Capture (EDC) systems, query management, and data cleaning processes, as well as practical experience with mock clinical trials and data management scenarios.
Certification
Recognized certification from a reputed institute adds credibility to your resume. Certifications demonstrate your proficiency in clinical data management to potential employers.
Career Advancement Opportunities
CDM training enhances your employability by equipping you with skills that are in high demand in the clinical research industry. Institutes often provide career counseling and guidance for entry-level roles such as Clinical Data Coordinator, Data Analyst, or Clinical Data Associate.
By embracing these innovations, clinical data management will not only become more efficient and effective but will also play a crucial role in advancing precision medicine and improving patient outcomes in clinical research.





